|
|
|
|
|
|
|
1. Spodick, DL. Acute Cardiac Tamponade. N Engl J Med 2003;349:684-90.
2.
Shabetai R. Pericardial effusion:
haemodynamic spectrum. Heart 2004;90(3): 255–256. |
|
2. JAMA 2007 Video: Large Pericardial Effusion With Tamponade And RV Collapse 3. From New York-Presbyterian: Review of apical echo views and tamponade.
4.
Large Pericardial Effusion Without
Tamponade.
6.
Determination Of Jugular Venous Pressure By
Physical Exam. |
|
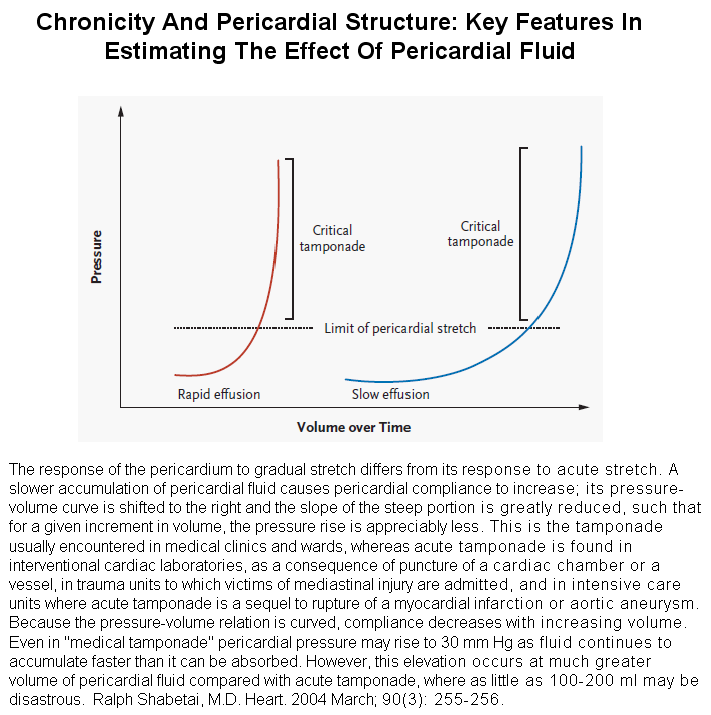
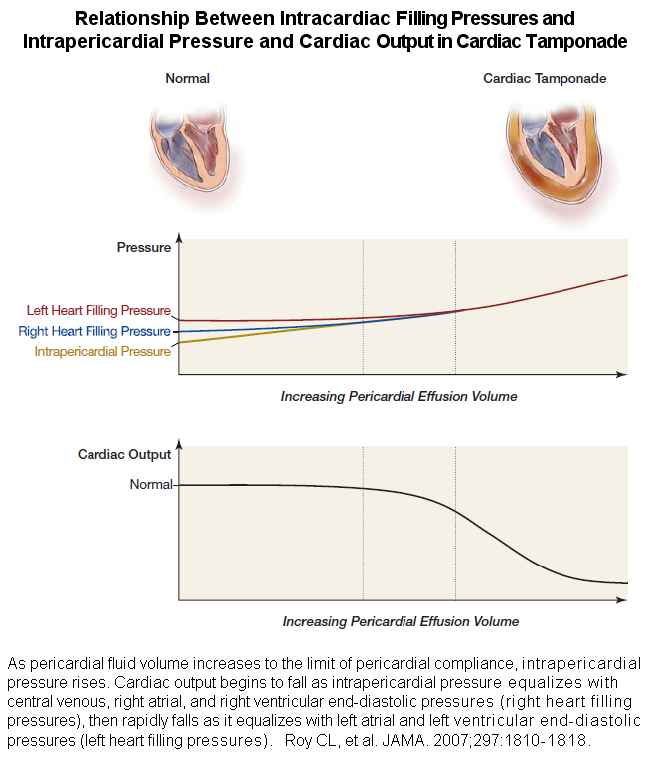
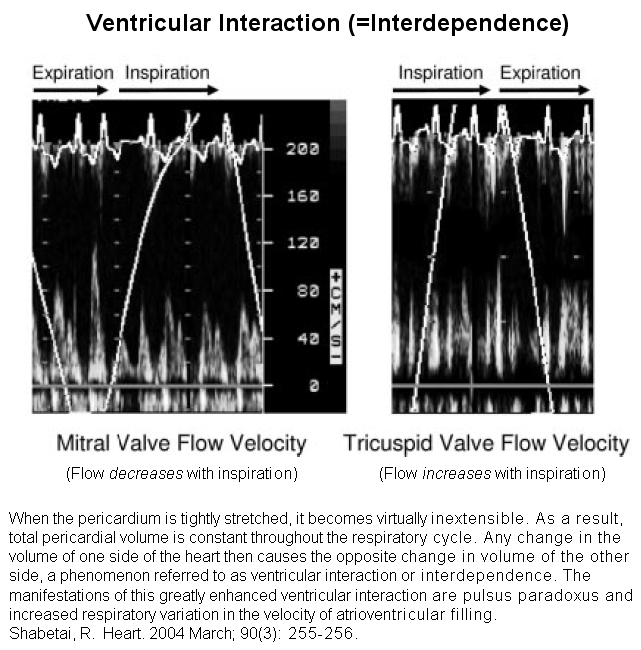
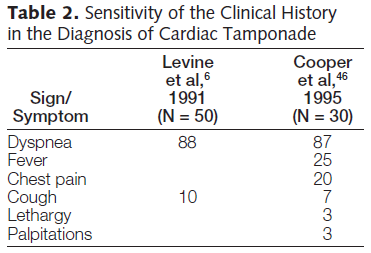
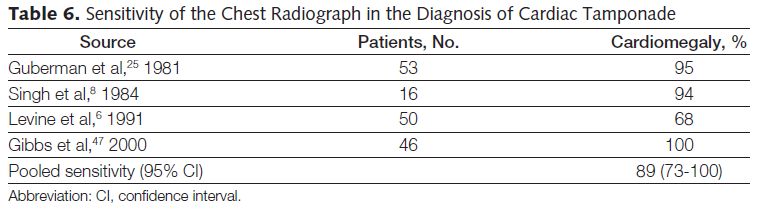
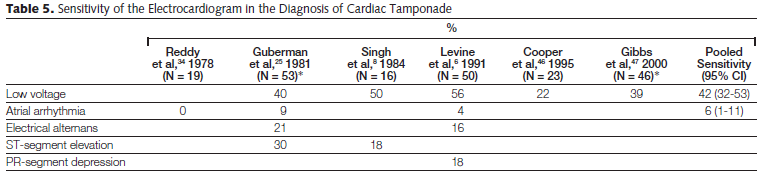
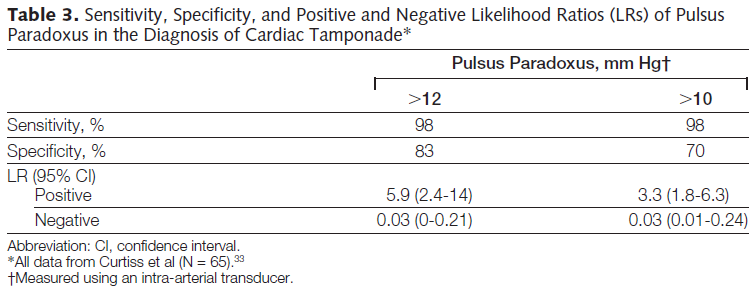
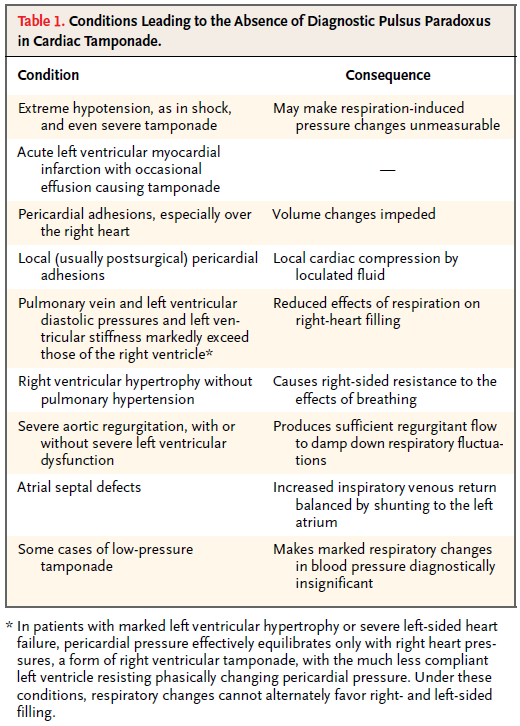
1. Diagnosis of cardiac tamponade can be easy, but only in advanced cases. 2. In all but advanced cases, cardiac tamponade would be most reliably diagnosed using measurement of pressures from all four cardiac chambers and the intrapericardial space. This approach, although accurate, would expose many patients to the hazards of needless procedures. 3. Dyspnea is the only symptom of cardiac tamponade with a high sensitivity, about 88%. Unfortunately, specificity of this symptom is low. 4. Pulsus paradoxus is the most useful physical finding in cardiac tamponade, with sensitivity of about 85% (range 71% to 98% in various studies) and specificity of about 76%. In unusual circumstances, pulsus paradoxus may be absent during cardiac tamponade. These include extreme hypotension, the presence of pericardial adhesions, severe right or left ventricular hypertrophy, atrial septal defect, severe aortic regurgitation and other unusual circumstances. (See Panel 8, on this Web page.) 5. Tachypnea (sensitivity = 80%), tachycardia (sensitivity = 77%) and elevated JVP (sensitivity = 76%) can also be helpful, but once again the specificity of each of these findings is low. 6. Echocardiographic markers of cardiac tamponade are also useful. Right atrial collapse has a sensitivity of 100%, but a specificity of only 33%, making it of very low utility. Right ventricular early diastolic collapse has a sensitivity of 75%, specificity of 85% and predictive value of 66%, which is helpful but by no means a certainty. 7. Other echocardiographic markers of cardiac tamponade are in much the same category. Respiratory variations >25-22% in mitral (falls with inspiration) and tricuspid (increases with inspiration) flow have a predictive accuracy of 73% and 64%, respectively. 8. The volume of pericardial fluid is of limited utility in making the diagnosis of cardiac tamponade, since very gradual accumulation (“medical effusion”) may result in a massive volume without much cardiac compression while very abrupt accumulation of pericardial fluid (“surgical/trauma/coronary angioplasty effusion”) may produce cardiac tamponade with as little as 100-200 ml of fluid. Similarly, even a slowly accumulating “medical” pericardial effusion may reach a tipping point at which addition of a small amount of fluid causes cardiac tamponade.
|
|
|